Angioplasty: The Malaysian Story
As we grow older, we tend to sit in the corner, and remember how life has been and had been. Some of us get an urge to record what happened for posterity.
Upon graduation from the University of Malaya in 1975, we were at the stage of staying congenital heart disease with the use of serial "park" films at University Hospital Kuala Lumpur (UHKL). The X-ray filming equipment was donated to us by the Americans and they sent Dr J.W. Kennedy (of LV cineangiogram LV function calculation fame), over to teach us how to do diagnostic studies on congenital heart disease. Dr J.W. Kennedy was very instrumental in developing cardiology in Malaysia. Besides me, Prof H.O. Wong, Dr K.T. Singham and Dr A. Masduki all benefitted from his training.
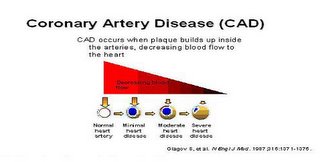
Our emphasis then was congenital and valvular heart disease, as these disease were then highly prevalent in Malaysia. It was closely linked to out pioneering cardiac surgery program in UHKL (that's another story). Coronary artery disease then was not a priority and no "coros" were done.
I left UHKL for Glasgow in 1977 to write my MRCP-UK. The present day trend of being offered a job by the host nation was prevalent then too. Upon completion an offer for a cardiology job in Glasgow Royal Infirmary was taken up and I trained under Dr Ross Lorimer and Dr Ian Hutton, in coronary arteriography.
At the same time Dr Nik Zainal was training in St Mary's Hospital to do coronary angiogram. While we were angiographing the Judkin's way they were , at St Mary's, doing "Coros " the Sone's way. He returned to HKL in 1980 to start the coronary program in HKL, and I rejoined UHKL the same year. At that time, Dr KT Singham was trying to start a coronary program, but the UHKL program was not as smooth as HKL, partly because of cardio-surgical facilities and interest and also personnel problems in UHKL.
There was no co-ordination between the HKL program and UHKL cardiology consultants. The early 1980's were also the dawn of angioplasty. Dr Gruentzig had done the first angioplasty in 1977 in Zurich, Switzerland, and Dr Richard Myler and Dr Simon Stertzer were also doing angioplasty in California. Some of our wealthier patients were being referred to the USA for angioplasty accompanied by some of our refering physicians on a fully paid basis when they flew with the patients.
Most of the patients then were referred to Dr Myler and Dr Stertzer in San Francisco Heart Center, in Seton City. Dr Sterzer would occasionally visit South East Asia to see some of his patients. On one of this visit to KL in 1982, he performed an angioplasty in UHKL. That was probably the very first angioplasty done in Malaysia. There was no attempt at a program but just the once a year case on the basis of the patient being a VIP who could pay. This went on for a while.
The equipment in UHKL was old and the film speed was hardly adequate for good quality coronary angiograms. There was no plan to start interventional cardiology although it was clearly gaining popularity in America and Europe. In 1983, Dr Gruenzig himself visited KL to give a talk to a packed audience. This was to be his last trip to KL as he met an untimely death in 1985 following an airplane crash. What a loss to the interventional world.
I struggled to get a coronary program started in UHKL without success. The obstruction was phenomenal. At that time the game in town was the occassional visitor swooping in and to do the occasional case, usually for VIPs, and that was it. This was an unthinkable way of doing things. All attempts were met with the response that medical lecturers should only teach and go on general medical calls. Ironically enough it was 1984 when I chose leave this Orwellian nightmare to join private practice. What a symbolic year.
In the interim I had been tracking the progress of angioplasty. There were training programs held regularly in the US. Most importantly, there were included "live cases", so that we could see and learn, through live transmission. That was 1988. The courses were well conducted and the registry data showed good success rates, with good symptom relief.
There was no reason Malaysia should be left out of the benefits of having an angioplasty program. In Jan 1988, I pulled together a small team, consisiting of a trained cardiologist from HKL (Ministry of Health), one from UKM (ministry of education) and myself (private practice), to go to San Francisco to attend a live demo course in April 1988, and then decide what was the best thing to do to bring the technique back to Malaysia.