Case Study - AZ
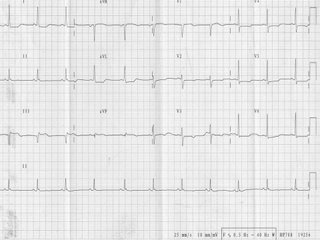
AZ, a 60 year old Malay male who has coronary risk factors of hypertension, NIDDM and smoking. He had been on regular follow up, the last being 1 month ago. He was apparently well till about 2 weeks ago when he noted occasional chest pains. On the day of presentation, he felt severe chest pains with severe cold sweat at about 9am. This slowly settled after an hour of rest and he continued to work. On reaching home, the chest pains recurred and he was persuaded to see a GP who refered him to the medical center. On presentation in the ER he had mild chest pains. His BP was 110/80mmHg and the HR was 90/min. Precordial examination was within normal limits and the lungs were clear. The ECG done is attached. Some blood test were also done.
Q1. What does the ECG show?
Q2. What is your provisional diagnosis?
Q3. How would you manage this patient if he had presented in your GP clinic?
Q4. How would you manage this patient in hospital?
2 comments:
1. SR, ST elevation in III and AVF, ST depression V2-V6.
2. Acute inferior STEMI.
3. Aspirin 300mg STAT. Plavix 300mg STAT. Call the reference hospital and refer STAT.
4. CCU admission. Rt sided ECG. IV Streptokinase. Others: IV Nitrate if persistent chest pain, Beta-blocker, ACEI, Statin, SC Insulin if sugar uncontrolled. May consider emergency PCI if feasible.
Q1. ST depression on anterior lateral leads (I, AVL, V2-V6), ST elevation in leads III and AVF (but not lead II?) and Q waves in III and V1 (physiological variant?).
This is suggestive of a progressive inferior myocardial infarct with ischaemia anterior laterally.
Q2. Progressive inferior AMI
Q3. Time of chest onset 9am.
Oxygen, high-flow (8L-10L) by mask.
Nitrates sublingual stat.
Morphine IV 5mg stat.
Aspirin 300mg stat + Clopidogrel.
LMWH/enoxaparin SC 1mg/kg if available --- heparin may help survival if neither thrombolysis or PCA is performed, or keeps things in stasis at least.
Beta-blocker, metoprolol, po.
Call for help: ambulance for closest tertiary centre with coronary intervention facilities.
Q4. 9am onset with Q waves (?>18 hours post?) but with on-going spread. Emergency referral to coronary care. Right-sided ECG and vitals (BP, pulse, Sat) monitoring. IV access. Meds as in Q3 (including high flow O2), tPA iv (tenectaplase) thrombolysis for on-going spread. Bloods: FBE with WCC differentials, urinalysis, cardiac enzymes, HbA1c.
Questions:
1. What are the guidelines for PCA? Is it 2 hours post, we use thrombolysis, otherwise, we use PCA if available within vicinity (based on door-to-needle versus door-to-stent time?)? What about for this case, where there seems to be on-going spread?
2. What is the notch after the QRS prominently seen in lead II called/what does it signify?
Thanks!
BTW, your reported HR is vastly different from the ~60bpm of the ECG, making me think that we should also check the name and date of the patient's ECG.
Post a Comment