Case study - AB
Mr AB is a 55yr old Malay male with a known history which was poorly controlled as he was poorly compliant. He does have occasional mild dizzy spells. He smokes and is overweight. Physical examination shows an obese male with a BMI of 30. His BP is 150/100mmHg and HR 80/min. Precordial examination is unremarkable. His (F) cholesterol is 6.3mMols/L, HDL-C is 0.9mMols/L, LDL-C is 4.5mMols/L, TG 3.5mMols/L, Sugar 6.4mMols/L. His renal function is normal. His ECG is attached.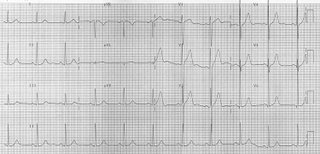
Q1. What is your diagnosis in this patient when he consults you?
Q2. How would you manage this patient?
Q3. How would you manage his dylipidemia?
Q4. Which is the drug of choice for controlling his hypertension?
No comments:
Post a Comment