Case Study - MR
MR is a 45yr old Indian gentleman, who presented to the emergency room of a general hospital at about 2100hrs with a complain of severe chest pains starting at about 1700hrs. He had initially thought that he was suffering from indigestion, but milk and food did not seem to help. When he begin to sweat and feel nauseous, his wife insisted that he consult a doctor. MR is a known hypertensive for the last 5 years and is on irregular treatment. He smokes and drinks alcohol. In ER, he was obviously tachypneic and restless, complaining of chest pains. He was cold and clammy with a BP of 90/60mmHg with a HR of about 110/min. There was a soft S3, and bibasilar lung crepitations. His ECG is attached.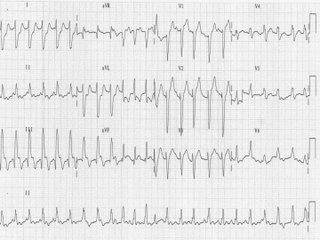
Q1. What is your clinical diagnosis?
Q2. How would you manage this patient?
Q3. How would you explain his illness to his wife, if she ask if he is in danger of death?
1 comment:
DX: Acute MI.
Tx:
Aspirin, Heparin, nitrates, O2.
Load with Plavix and send to cath lab immediately if available.
Otherwise TPA if no contraindications exist.
Also start statin during admission based on recent trial results.
Post a Comment